At Alice’s Psychiatry and Wellness, we understand the challenges of finding effective depression treatments. TMS treatment for depression has emerged as a promising option for many patients.
This blog post will guide you through the process of choosing TMS therapy, covering its effectiveness, key factors to consider, and what to expect during treatment.
What is TMS and How Does It Work?
Understanding Transcranial Magnetic Stimulation
Transcranial Magnetic Stimulation (TMS) is a non-invasive treatment that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of major depression. This innovative approach has shown promising results for patients struggling with depression, especially when other treatments haven’t worked.
The Science Behind TMS
TMS targets the dorsolateral prefrontal cortex, a region of the brain linked to mood control. The treatment delivers magnetic pulses to activate brain cells, which may improve neural connectivity and neurotransmitter function. Unlike electroconvulsive therapy (ECT), TMS doesn’t require anesthesia and has fewer side effects.
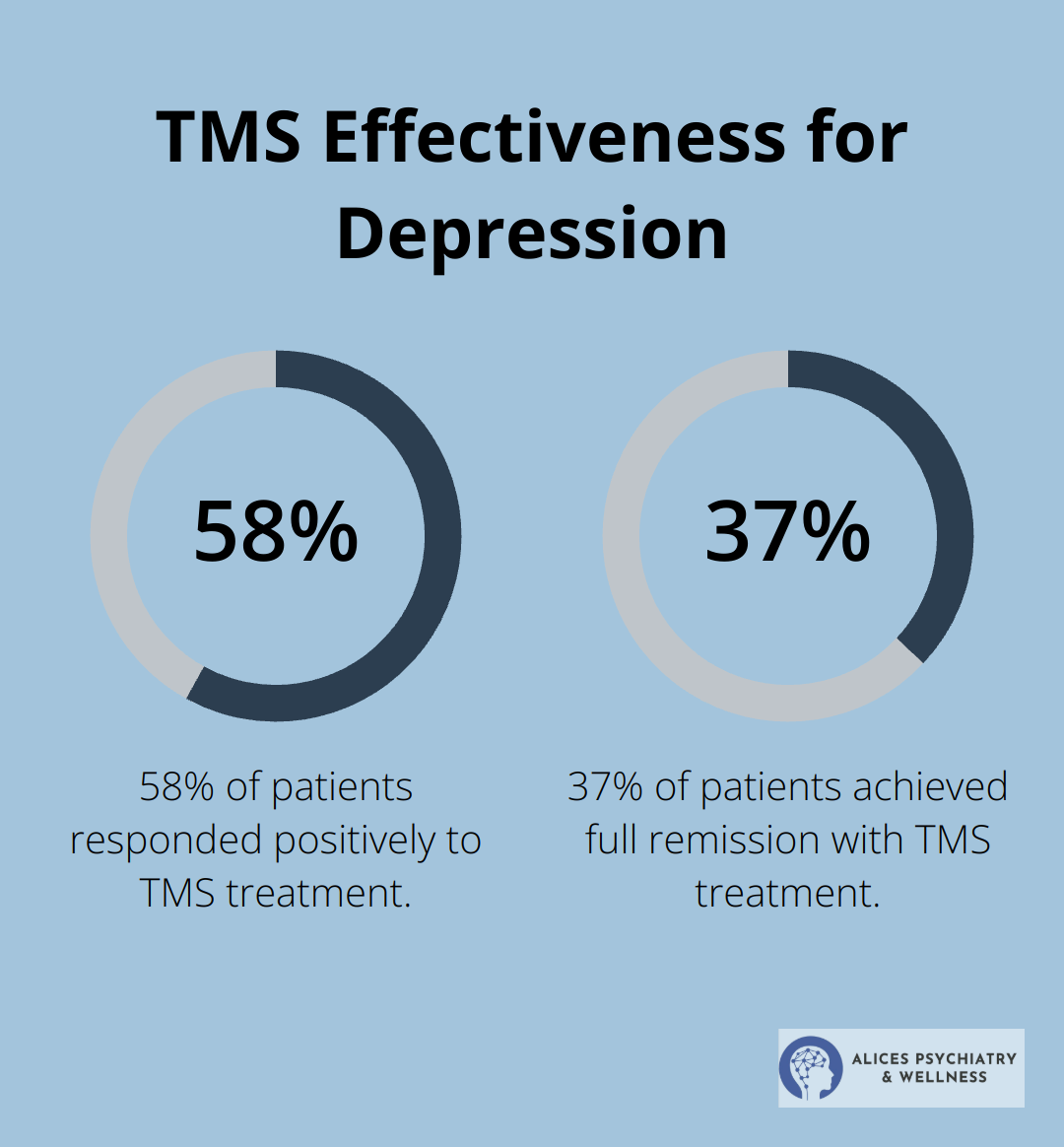
TMS Effectiveness for Depression
Research supports the efficacy of TMS in treating depression. A 2015 study published in the Journal of Clinical Psychiatry revealed impressive results: 58% of patients responded positively to TMS, with 37% achieving full remission. These outcomes are particularly noteworthy considering that TMS is often used for treatment-resistant depression (cases where other treatments have failed).
TMS vs. Traditional Treatments
TMS offers several advantages over conventional depression treatments:
- Medication Comparison: Unlike antidepressants, TMS doesn’t cause weight gain, sexual dysfunction, or other systemic side effects. It’s also more targeted than medications, which affect the entire body.
- Psychotherapy Contrast: While therapy remains crucial for long-term mental health, TMS can provide faster relief for some patients (often within weeks).
- ECT Alternative: TMS is less invasive than ECT and doesn’t require general anesthesia or cause memory loss.
Personalized Approach to TMS
It’s important to note that TMS isn’t a one-size-fits-all solution. Some patients may benefit more from a combination of treatments. A thorough evaluation (including medical history and previous treatment responses) is essential to determine if TMS is the right approach for each individual.
As we move forward, let’s explore the key factors to consider when choosing TMS treatment for depression. Understanding these elements will help you make an informed decision about whether TMS might be the right option for your mental health journey.
Key Factors in Choosing TMS Treatment
Assessing Depression Severity
The severity of your depression symptoms significantly influences whether TMS is the right choice. A study published in the Journal of Affective Disorders in 2023 revealed that patients with moderate to severe depression showed the most substantial improvement with TMS therapy. If persistent symptoms interfere with your daily life, TMS might be a viable option for you.
Evaluating Past Treatment Responses
Your history with other depression treatments is a critical factor. Repetitive transcranial magnetic stimulation augmentation was shown to be more effective than switching antidepressants in treatment-resistant depression. If you’ve tried multiple medications or therapies without success (or with limited success), TMS could offer a new avenue for relief.
Understanding Medical Considerations
Certain medical conditions or implants can affect your eligibility for TMS. For instance, the presence of metal implants in the head or neck area, a history of seizures, or pregnancy may preclude TMS treatment. A comprehensive medical evaluation is essential to ensure TMS is safe for you.
Navigating Financial Aspects
While TMS is increasingly covered by insurance plans, it’s important to understand your coverage. A 2024 policy update affecting over 15 million covered lives through BCBS Illinois, BCBS Montana, BCBS New Mexico, and other states, indicates growing insurance coverage for TMS treatment. However, out-of-pocket costs can vary. We recommend you contact your insurance provider to discuss coverage details and explore potential financial assistance programs if needed.
Choosing a TMS Provider
The selection of a TMS provider is a key factor in your treatment journey. Look for providers with extensive experience in administering TMS therapy and a track record of successful outcomes. Consider factors such as the provider’s qualifications, the technology they use, and their approach to personalized care.
When you weigh these factors, it’s important to consult with a mental health professional who can provide personalized guidance. A comprehensive evaluation will help determine if TMS is the right path for your mental health journey. Your unique circumstances should be considered to develop a treatment plan tailored to your needs, ensuring you receive the most effective care possible.

As we move forward, let’s explore what you can expect during the TMS treatment process, from initial consultation to completion of therapy.
What Happens During TMS Treatment?
Initial Consultation and Evaluation
Your Transcranial Magnetic Stimulation (TMS) journey starts with a comprehensive evaluation. A mental health professional will review your medical history, current symptoms, and previous treatments. This step determines if TMS suits you and creates a personalized treatment plan.
The evaluation includes standardized depression assessments, such as the Hamilton Depression Rating Scale (HAM-D) or the Beck Depression Inventory (BDI). These tools establish a baseline for your symptoms and track progress throughout treatment.
Treatment Schedule and Duration
TMS therapy involves a series of sessions over several weeks. A typical course of treatment includes:
- 5 sessions per week (Monday through Friday)
- 4 to 6 weeks of treatment
- Each session lasts about 20 to 40 minutes
This intensive schedule allows for consistent brain stimulation, which is key to the treatment’s effectiveness. Research shows that patients who complete the full course of TMS treatment have significantly better outcomes than those who don’t.

The TMS Session Experience
During a TMS session, you sit comfortably in a chair while a technician positions the magnetic coil against your head. You’ll hear clicking sounds and feel a tapping sensation on your scalp as the magnetic pulses are delivered. Many patients describe the sensation as mild and tolerable.
You remain awake and alert throughout the session. You can even listen to music or watch TV during treatment. After each session, you can immediately return to your daily activities (including driving).
Managing Side Effects
TMS is generally well-tolerated, with fewer side effects compared to many antidepressant medications. However, some patients may experience:
- Mild headache
- Scalp discomfort at the treatment site
- Lightheadedness
These side effects typically subside after the first few sessions as your body adjusts to the treatment. Mental health professionals closely monitor patients and provide strategies to manage any discomfort, such as over-the-counter pain relievers or adjustments to the stimulation intensity.
Serious side effects, such as seizures, are extremely rare.
Throughout your TMS treatment, mental health professionals will regularly assess your progress and adjust the treatment plan as needed. Many patients start noticing improvements in their mood and energy levels after 2 to 3 weeks of treatment, although individual experiences may vary.
TMS is just one part of a comprehensive approach to managing depression. Mental health professionals often recommend combining TMS with other therapies (such as cognitive-behavioral therapy or medication management) for optimal results.
Final Thoughts
TMS treatment for depression offers a promising alternative for patients who struggle with traditional therapies. This non-invasive approach has shown significant effectiveness, especially for treatment-resistant cases. When you consider TMS, you must evaluate factors such as symptom severity, treatment history, and potential medical contraindications.
The TMS treatment journey involves a comprehensive evaluation, followed by a series of sessions over several weeks. Many patients find the potential benefits outweigh the time investment, with generally mild side effects and the ability to resume daily activities immediately after each session. Every individual’s mental health journey is unique, so you should consult with a qualified mental health professional to determine if TMS is right for you.
If you want to explore TMS treatment for depression, we at Alice’s Psychiatry and Wellness can support you. Our team of experienced mental health professionals provides comprehensive evaluations and personalized treatment plans. We offer a range of services to complement TMS treatment if appropriate, with the goal to empower you on your journey to mental wellness.





