Depression affects millions worldwide, and finding the right treatment can be overwhelming. At Alice’s Psychiatry and Wellness, we understand the complexities of this condition and the importance of comprehensive care.
Depression treatment programs offer a structured approach to managing symptoms and improving overall well-being. This blog post will explore the key components of effective programs and how they can help individuals on their path to recovery.
Understanding Depression Treatment Programs
Depression treatment programs offer structured approaches to help individuals manage and overcome depression. These programs come in various forms, each catering to different levels of care and individual needs.
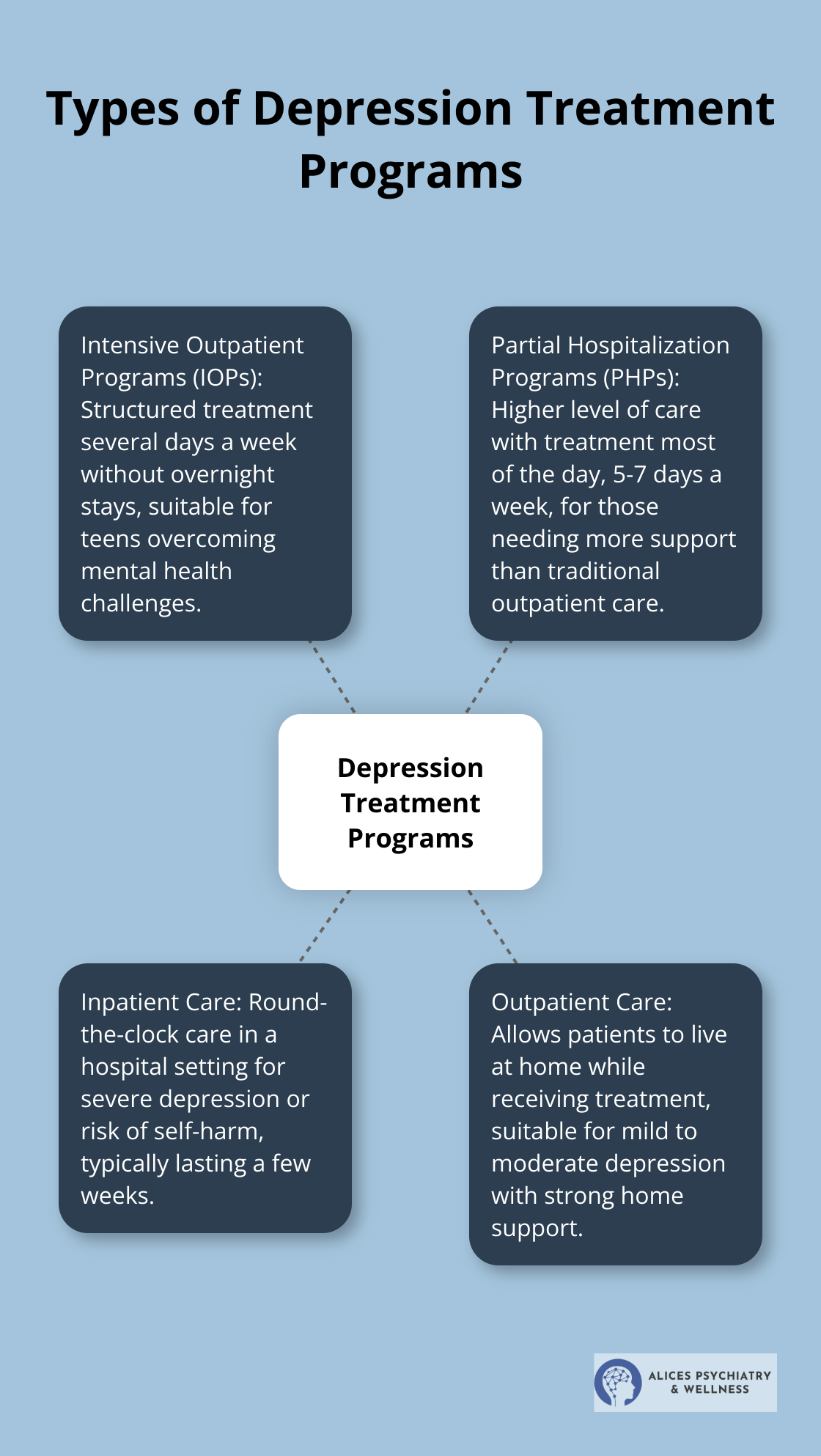
Types of Depression Treatment Programs
Intensive outpatient programs (IOPs) provide structured treatment several days a week without requiring overnight stays. These programs can support teens in overcoming mental health challenges today. Partial hospitalization programs (PHPs) offer a higher level of care, with patients attending treatment for most of the day, five to seven days a week. PHPs suit those who need more support than traditional outpatient care but don’t require 24-hour supervision.
Inpatient vs. Outpatient Care
The choice between inpatient and outpatient care depends on the severity of depression and the individual’s circumstances. Inpatient programs provide round-the-clock care in a hospital setting, ideal for those with severe depression or at risk of self-harm. These programs typically last for a few weeks and focus on stabilization and intensive treatment. Outpatient programs allow patients to live at home while receiving treatment. This option suits those with mild to moderate depression who have a strong support system at home.
Personalized Treatment Plans
Personalized treatment plans address specific symptoms, triggers, and goals. A comprehensive evaluation (including psychological tests, medical examinations, and discussions about personal history) forms the first step in creating an effective treatment plan.
These plans often combine various therapeutic approaches. Cognitive Behavioral Therapy (CBT) helps patients identify and change negative thought patterns. Other evidence-based therapies like Interpersonal Therapy (IPT) or Dialectical Behavior Therapy (DBT) may be incorporated based on individual needs. Medication management often plays a key role in treatment, with options ranging from selective serotonin reuptake inhibitors (SSRIs) to newer treatments like ketamine therapy for treatment-resistant depression.
Holistic Approaches
Many depression treatment programs now incorporate holistic approaches to complement traditional therapies. These may include mindfulness practices, yoga, art therapy, or nutritional counseling. Such approaches (often referred to as “complementary therapies”) can help patients develop coping skills, reduce stress, and improve overall well-being.
Measuring Progress and Adjusting Treatment
Effective depression treatment programs continuously monitor patient progress and adjust treatment as needed. This may involve regular assessments using standardized tools (such as the Patient Health Questionnaire-9 or PHQ-9), feedback from the patient and their support network, and ongoing discussions with the treatment team. This dynamic approach ensures that the treatment remains responsive to the patient’s changing needs and circumstances.
As we explore the key components of effective depression treatment in the next section, we’ll delve deeper into the specific therapies and interventions that form the backbone of comprehensive care.
What Makes Depression Treatment Effective?
Medication Management: A Foundation for Recovery
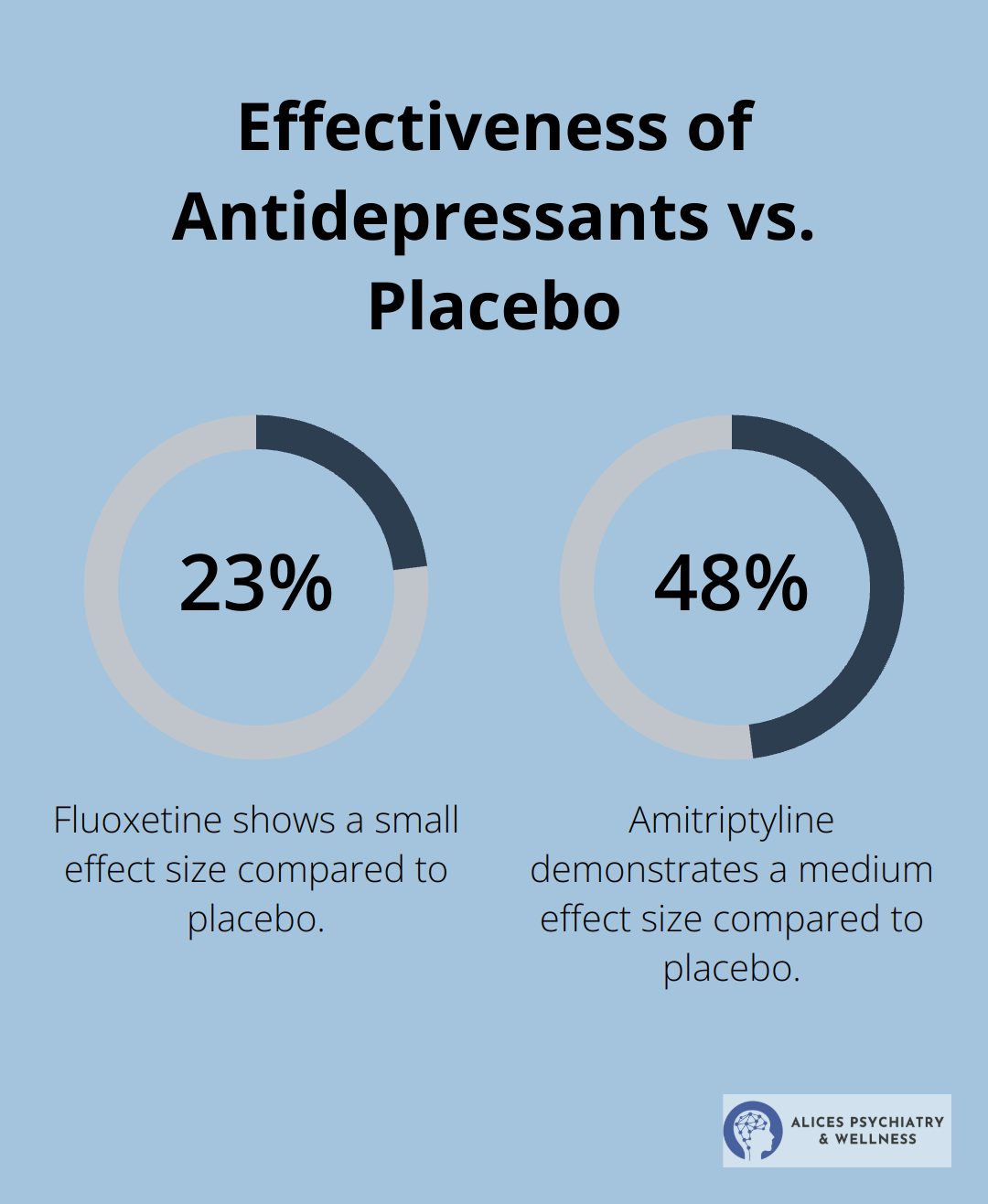
Antidepressants form a cornerstone in managing depression symptoms for many individuals. A 2021 Lancet study revealed that antidepressants show small to medium-sized effects compared to placebo (standardized mean differences range from 0.23 for fluoxetine to 0.48 for amitriptyline). However, finding the right medication requires patience and careful monitoring.
Pharmacogenetic testing helps determine which medications may work best based on a patient’s genetic makeup. This approach can enhance remission and response rates, potentially reducing the trial-and-error process and leading to more effective treatment outcomes.
Therapy: Transforming Thoughts and Behaviors
Individual and group therapy sessions form the backbone of many depression treatment programs. Cognitive Behavioral Therapy (CBT) has shown particularly promising results. Other evidence-based approaches like Interpersonal Therapy (IPT) and Dialectical Behavior Therapy (DBT) can also prove highly effective, depending on the individual’s needs and circumstances. The key lies in finding the right therapeutic approach that resonates with each patient.
Lifestyle Modifications: Small Changes, Big Impact
While medication and therapy form the core of depression treatment, lifestyle modifications can significantly enhance their effectiveness. Regular exercise, for instance, has shown antidepressant effects. A systematic review published in the Journal of Affective Disorders in 2021 found that structured exercise proves more effective when combined with other treatments than on its own.
Nutrition plays a vital role as well. Some studies suggest that dietary supplements (like omega-3 fatty acids and probiotics) may modestly improve symptoms when used alongside traditional treatments. However, it’s essential to consult with a healthcare provider before starting any supplement regimen.
Sleep hygiene represents another critical aspect of depression management. Establishing a consistent sleep schedule and creating a relaxing bedtime routine can help improve mood and energy levels.
Holistic Approaches: Complementing Traditional Therapies
Many depression treatment programs now incorporate holistic approaches to complement traditional therapies. These may include mindfulness practices, yoga, art therapy, or nutritional counseling. Such approaches (often referred to as “complementary therapies”) can help patients develop coping skills, reduce stress, and improve overall well-being.
Continuous Monitoring and Adjustment
Effective depression treatment programs continuously monitor patient progress and adjust treatment as needed. This may involve regular assessments using standardized tools (such as the Patient Health Questionnaire-9 or PHQ-9), feedback from the patient and their support network, and ongoing discussions with the treatment team. This dynamic approach ensures that the treatment remains responsive to the patient’s changing needs and circumstances.
As we move forward, we’ll explore how success in depression treatment programs is measured and the importance of ongoing support in maintaining long-term mental health.
How We Measure Success in Depression Treatment
Quantitative Assessment Tools
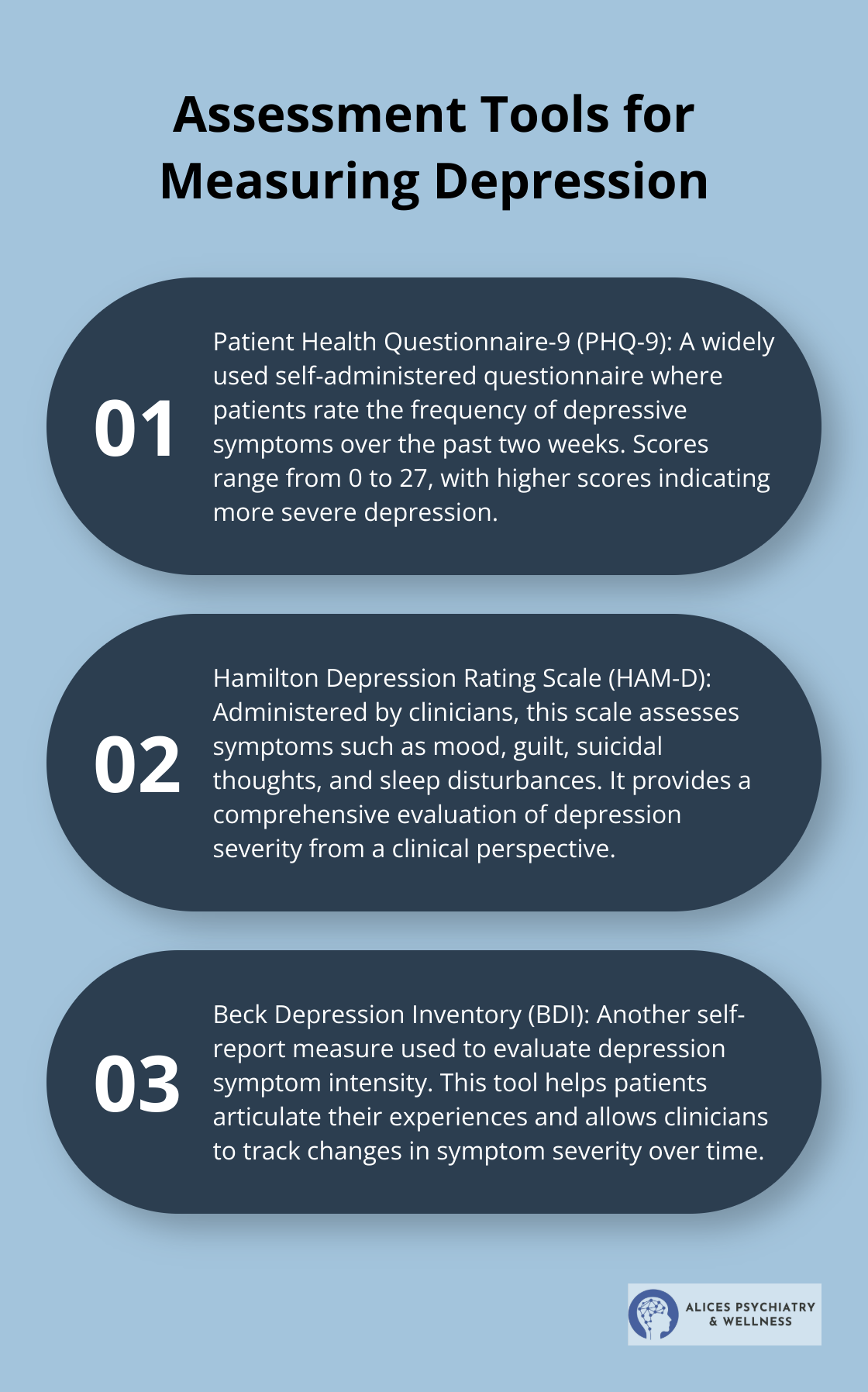
We use several standardized tools to measure depression severity and treatment progress. This study is the first to use PHQ-9 and HAMD-17 to explore the discrepancies between self and observer rated depression. The Patient Health Questionnaire-9 (PHQ-9) stands out as a widely used self-administered questionnaire. Patients rate the frequency of depressive symptoms over the past two weeks, with scores ranging from 0 to 27 (higher scores indicate more severe depression).
The Hamilton Depression Rating Scale (HAM-D), administered by clinicians, assesses symptoms such as mood, guilt, suicidal thoughts, and sleep disturbances. The Beck Depression Inventory (BDI) provides another self-report measure to evaluate depression symptom intensity.
Qualitative Measures of Progress
Quantitative tools provide valuable data, but they don’t tell the whole story. We focus on qualitative measures of progress, such as improvements in daily functioning, relationships, and overall quality of life. These aspects come to light through ongoing conversations with patients and their support networks.
We track a patient’s ability to return to work, engage in social activities, or pursue once-enjoyed hobbies. These real-world indicators of improvement often prove just as important as changes in symptom scores.
Short-Term vs. Long-Term Outcomes
Short-term outcomes typically focus on symptom reduction and crisis management.
Long-term outcomes hold equal importance.
We try to achieve sustained remission. Remission is a phase on the path of depression treatment that comes after a major depressive episode. We also track relapse rates and work with patients to develop strategies for maintaining their mental health over the long term.
The Role of Ongoing Support and Follow-Up Care
Successful depression treatment doesn’t end when symptoms improve. Ongoing support and follow-up care play a vital role in maintaining progress and preventing relapse.
We implement a structured follow-up schedule, with more frequent check-ins immediately after treatment initiation or major changes. This approach allows us to catch any signs of relapse early and adjust treatment as needed.
We encourage patients to engage in ongoing self-monitoring and to reach out if they notice concerning changes in their mood or functioning. This proactive approach helps prevent minor setbacks from escalating into major depressive episodes.
Final Thoughts
Depression treatment programs offer a comprehensive approach to manage this complex mental health condition. These programs combine medication management, therapy sessions, and lifestyle modifications to address depression’s multifaceted nature. Evidence-based approaches like Cognitive Behavioral Therapy and holistic treatments provide well-rounded care tailored to individual needs.
The effectiveness of depression treatment programs depends on personalized care plans and continuous monitoring. Success is measured through quantitative assessments and qualitative improvements in daily functioning (and overall quality of life). Both short-term symptom relief and long-term maintenance of mental health play important roles in successful treatment.
Professional help is a critical step for anyone struggling with depression. Alice’s Psychiatry and Wellness offers personalized treatment plans to support individuals on their wellness journey. Our team of experienced mental health professionals provides compassionate care, utilizing advanced methods to optimize treatment outcomes.





